Cigarettes, Health
Can I Smoke Cigarettes While on Antidepressants?
Cigarette smoking provides a number of calming effects to smokers. One reason behind this is nicotine, which is naturally produced by the tobacco smoke from cigarettes. Nicotine is a highly addictive substance that can reach your brain as quickly as possible. As the cigarette smoke enters the lungs, its nicotine content is being absorbed. This substance then travels to the brain within seconds, which triggers the release of dopamine and other neurotransmitters that cause a buzz or feeling of pleasure, concentration, and relaxation. The soothing effects of cigarettes typically entice individuals who might be experiencing stress, anxiety, or even depression. Those who take antidepressants and other similar medications might also want to smoke cigarettes due to their effects. But is it a good move to smoke cigarettes while on antidepressant drug treatment? Find out more here at Native Smokes 4 Less.
Introduction to Antidepressants
If you have depression, you have to take antidepressants to help treat the said mood disorder. Depression is a mood disorder that causes a persistent feeling of sadness as well as a loss of interest in activities and things you once enjoyed fully. It may likewise cause difficulty with thinking, motivation, eating, sleeping, and even memory.
Not all depressive disorders are similar. They come in many types, including clinical depression (major depressive disorder), bipolar depression, persistent depressive disorder (PDD), premenstrual dysphoric disorder (PMDD), atypical depression, and seasonal depression (seasonal affective disorder). To treat depression, healthcare providers typically prescribe antidepressants. Some particular conditions that antidepressants may be able to treat include clinical depression and other depressive disorders, bipolar disorder, bulimia, generalized anxiety disorder (GAD), obsessive-compulsive disorder (OCD), panic disorder, post-traumatic stress disorder (PTSD), and social anxiety disorder (social phobia).A number of healthcare providers then prescribe these medications for chronic pain, insomnia, and migraine. This type of prescription is typically considered an off-label use of the medication.
The working principles of antidepressants are pretty straightforward.They typically alter the way your brain uses neurotransmitters to effectively regulate your behaviour and mood. The most common brain chemicals or neurotransmitters that antidepressants often regulate include serotonin, norepinephrine, and dopamine.
Aside from changing the way your brain works, antidepressant treatments can also induce neuroplasticity. It is a process wherein your brain changes its structure by strengthening or weakening connections between neurons or brain cells.While antidepressants, regardless of their class or type, can treat a number of symptoms of the said mood disorder, these medications might not be able to address its causes. A number of studies show that the effectiveness of antidepressant treatment can often depend on the severity of the depression. In moderate, severe, and chronic depression, antidepressants are typically effective. Those with mild depression, alternatively, might not be able to benefit from antidepressants.Given this fact, medical professionals often recommend pairing antidepressant treatment with psychotherapy or talk therapy. The combination of these two things can typically produce the largest improvements in depression symptoms.
The Relationship Between Smoking and Depression Pharmacological Treatment
The complex relationship between smoking and depression has significant implications for pharmacological treatment. Many adults, especially those who are depressed and taking depression pharmacological treatment, smoke cigarettes as their primary way of coping with the feelings or emotions they are dealing with. Additionally, they believe that smoking can alleviate their depressive symptoms temporarily. They likewise depend on nicotine and its calming effects.
Nicotine, the primary addictive component in tobacco, interacts with brain chemistry in ways that can alleviate depressive symptoms in a short time by stimulating the release of dopamine, serotonin, and norepinephrine. However, this relief is short-lived. So, over time, nicotine dependence can worsen mental health, which contributes to a cyclical pattern of low mood and smoking.
From a pharmacological standpoint, smoking introduces tons of complications in treating depression.One of the key issues is the way smoking affects the metabolism of antidepressant medications. Cigarette smoke contains substances such as polycyclic aromatic hydrocarbons that induce liver enzymes, particularly cytochrome P450 1A2 (CYP1A2). This enzyme is responsible for metabolizing several antidepressants, including fluvoxamine, duloxetine, mirtazapine, tricyclic antidepressants (TCAs), benzodiazepines, clozapine, and olanzapine.
In individuals who smoke, these types of antidepressants may be broken down more rapidly, which leads to reduced plasma concentrations and reduced therapeutic effects. Healthcare professionals may prescribe higher doses to compensate for the increased metabolic rate. However, it only creates a delicate balancing act. If the patient quits smoking suddenly, the same dosage could result in toxic drug levels, which increase the risk of adverse side effects.
Moreover, smoking reduces the levels of monoamine oxidase (MAO) enzymes in the brain that help break down neurotransmitters. This reduction mimics the effect of a number of antidepressant medications and will only complicate treatment outcomes.
Most antidepressants, after all, could cause side effects that depend on the dose taken. Some side effects could only occur when the levels of the antidepressant in the blood reach a certain point. Since smoking tobacco can decrease the levels of some drugs in the blood, quitting smoking, especially for heavy smokers who take these medications, could increase the intensity of these drugs. This increase might cause side effects that were not present before.
For depression, smoking cessation must be considered a vital component of a comprehensive treatment plan. Quitting smoking, however, could be particularly challenging for those with existing mental health conditions. Withdrawal symptoms like irritability, low mood, and anxiety may only worsen depressive symptoms in the short term.
Nonetheless, research suggests that successful long-term smoking cessation is directly linked with improved mood and reduced symptoms of depression. Therefore, it’s important for a doctor to create a well-structured cessation strategy to account for the mental health status of patients with depression.
When it comes to pharmacological aids for smoking cessation, bupropion is notable for its dual role. It is not only an antidepressant but also approved as a smoking cessation aid. Its dual function makes it particularly suitable for patients dealing with both nicotine dependence and depression.
Another option is varenicline, which has been shown to be effective in promoting smoking cessation. However, there have been concerns about its potential to elevate psychiatric symptoms, although more recent studies indicate that it is safe when properly monitored.
Integrating smoking cessation support with mental health is vital, benefitting patients who find it difficult to quit smoking while dealing with depression or other mental health issues. A coordinated approach that involves general practitioners, psychiatrists, and cessation specialists is then important so they can craft an integrated care model that lets them monitor medication interactions and adjust the dosage, especially if a patient decides to reduce or quit smoking during the course of treatment.
Depression treatment among smokers can be a complex but manageable task, especially when approached with a full understanding of how tobacco smoke affects pharmacological outcomes. Fortunately, they can expect better health outcomes if their medications have been adjusted based on their smoking status and habit if their cessation aids like nicotine replacement therapy tools (NRTs) have been carefully selected, and if they continuously receive psychological support.
Types of Antidepressants
Antidepressants were invented in the 1950s. Since then, researchers have developed several variations of the said drugs to cater to as many patients with depression as possible.Some types or classes of antidepressants include:
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin/norepinephrine reuptake inhibitors (SNRIs)
- Tricyclic antidepressants (TCAs)
- Atypical antidepressants
- Serotonin modulators
- Monoamine oxidase inhibitors (MAOIs)
- N-methyl-D-aspartate (NMDA) antagonists
The most common type of prescribed antidepressant today is SSRIs. One of the most well-known SSRIs you can buy today is Fluoxetine (Prozac).
TCAs, alternatively, are only reserved for treatment-resistant depression and anxiety since they pose an increased rate of side effects. The oldest antidepressant drug treatment available today is MAOIs. Even though they are highly effective, they are only meant for treatment-resistant anxiety and depression since they require dietary modifications that can help avoid hypertensive reactions. Most of the time, antidepressants come in pill or tablet form. If you’re prescribed antidepressant treatment, you should swallow the pills with a liquid, like water.
When it’s your first time taking an antidepressant, your doctor will likely prescribe the lowest possible dose of antidepressant treatment that they think is needed to improve your symptoms. They’ll eventually adjust the dose if necessary. Usually, it would take you numerous weeks before you start experiencing an improvement in your symptoms.
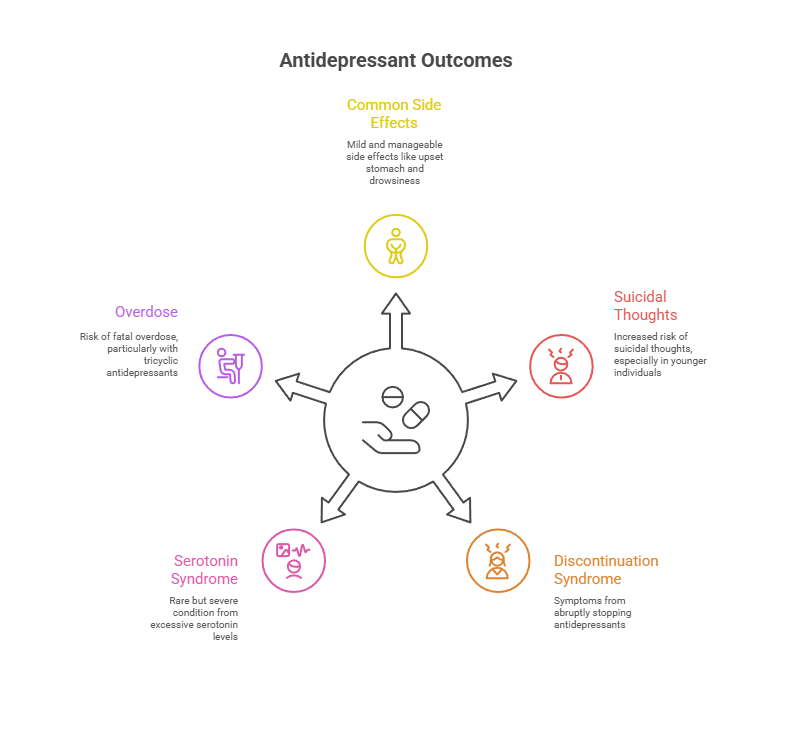
Once you begin to feel better, your treatment may last at least six months. However, if you experience recurrent, chronic, or severe depression, your healthcare professional may recommend continuing antidepressant treatment indefinitely.It’s important to note that taking antidepressants may cause a number of side effects. Some common side effects of taking antidepressants include:
- Upset stomach
- Diarrhea
- Headache
- Drowsiness
- Sexual dysfunction
These side effects are often mild and can improve with time. If you experience unpleasant side effects from taking antidepressants, you should talk to your healthcare provider. They may recommend adjusting your dose or opting for a different type or class of medication.
Aside from side effects, taking antidepressants may likewise cause a number of complications. Four possible complications of using antidepressants include the following:
- Suicidal thoughts or behaviour: On a number of occasions, those under the age of 25, including children and adolescents, may encounter an increase in suicidal thoughts or behaviour following the start of taking antidepressants or adjusting to a new dose of the medicine. Should you or your loved one manifest suicidal thoughts or behaviour, you should contact the healthcare professional who prescribed the medication right away.
- Antidepressant discontinuation syndrome: Antidepressant discontinuation syndrome may occur if you abruptly stop taking your antidepressants after at least six weeks of continuous use. Some symptoms of antidepressant discontinuation syndrome include flu-like symptoms like fatigue, headache, muscle aches, sweating, insomnia, nausea, dizziness and lightheadedness, sensory issues like burning, tingling, or shock-like sensations, anxiety, irritability and agitation. These symptoms are typically mild but can be uncomfortable, and can persist for one to two weeks.
- Serotonin syndrome: Serotonin syndrome is a rare yet potentially life-threatening drug reaction that occurs when the body accumulates excessive serotonin levels. It can manifest when individuals commence a new antidepressant or increase their existing dosage. If your body’s serotonin processing mechanisms differ or cannot handle an increased serotonin intake, this syndrome can eventually develop. Some symptoms of serotonin syndrome include nervousness, nausea and vomiting, diarrhea, dilated pupils, and muscle issues, including twitching, involuntary contractions, spasms, rigidity, sweating and shivering, and side-to-side eye movements. Severe symptoms of this syndrome include confusion or delirium, rapid heart rate (tachycardia), high blood pressure, fever, seizures, and loss of consciousness.
- Overdose: Antidepressants can vary widely in terms of their toxicity. Tricyclic antidepressants, unfortunately, pose the highest risk of fatality when taken in overdose. Some signs and symptoms of tricyclic antidepressant overdose include heart rhythm disturbances, low blood pressure, drowsiness, rigid muscles, mental confusion, and coma. Now, it’s highly important to discuss the risk of overdose with your healthcare provider or pharmacist. Additionally, you must adhere to your medication’s prescribed dosage. If you suspect an overdose, whether in yourself or a loved one, you should seek immediate medical attention.
Just like the side effects of antidepressants, you should consult your doctor if you experience these complications and their accompanying symptoms.
Interactions Between Antidepressants and Smoking
A lot of cigarettes are being offered in online stores and tobacco shops today. Native Smokes 4 Less, for instance, sells a wide range of premium cigarettes from varying brands at great prices.
Cigarettes, regardless of their type, brand, or flavour, can cause a number of health risks that a lot of you might be already familiar with.These health risks include cancer, lung disease, heart disease, stroke, chronic respiratory conditions, diabetes, and dental problems. Another effect of smoking cigarettes, however, is it can decrease the efficacy of many medications, particularly those needed for various psychiatric disorders.Tobacco smoke from cigarettes induces many of the CYP450 enzymes in the liver. These enzymes play a key role in medication absorption, distribution, metabolism, and elimination. The interactions with drugs are mainly caused by the tobacco smoke components, rather than nicotine. Therefore, NRT can be used without worrying about drug interactions and changes in medications. Many psychiatric medications could be affected by cigarette smoking. They include antipsychotics, antidepressants, hypnotics, and anxiolytics. The drug concentration in the blood for these classes may be reduced with smoking. Reduction in efficacy may, unfortunately, lead to inappropriate adjustments of medications to higher dosages.
If a patient is smoking and is taking a medication that is negatively affected by cigarettes, their pharmacist should initiate a smoking cessation regimen or NRT. It’s important to note that smoking cessation or NRT can harm the patient in the short term since abruptly stopping cigarette smoking can make them feel uncomfortable due to the existence of withdrawal symptoms.
Since a number of medications are typically dosed with consideration that the patient is a cigarette smoker, it’s vital to make the right dosage adjustments when trying to initiate and implement smoking cessation measures. A specific CYP450 enzyme induced by smoking cigarettes is CYP1A2. This enzyme is responsible for metabolizing several antidepressants, which include TCAs like nortriptyline and imipramine, as well as certain SSRIs, such as fluvoxamine. In smokers, the increased activity of this particular enzyme accelerates the breakdown of these medications, which results in lower blood plasma concentrations and diminished therapeutic effects.
For instance, if you’re a smoker who is taking fluvoxamine, you may experience suboptimal symptom relief, even at standard doses, since the medication is metabolized too quickly to maintain steady therapeutic levels. To address this, you must be prescribed by your doctor with higher doses, but this introduces risks, especially if you suddenly quit smoking.
When smoking stops, CYP1A2 activity gradually returns to normal levels, which slows down drug metabolism and potentially leads to elevated concentrations that increase the likelihood of side effects such as sedation, dizziness, or gastrointestinal issues.
Nicotine and antidepressants interact pharmacologically, which adds another layer of complexity to their treatment. This overlap can blur the lines between medication response and nicotine’s psychoactive effects, which makes it difficult to determine if an improvement in mood is due to pharmacotherapy or nicotine consumption.
Furthermore, relying on nicotine to regulate mood can interfere with the therapeutic process, which delays or masks progress in treating depression and other similar disorders.
And as discussed earlier, smoking also alters the brain’s MAO activity. MAO enzymes degrade neurotransmitters, and smoking suppresses MAO levels in the brain, mimicking the effect of MAO inhibitors, a class of antidepressants.While this may seem beneficial, it creates an unstable chemical environment that complicates pharmacological intervention. When antidepressants are added to this altered baseline, their expected effects might not occur as predicted.
These interactions are particularly important during smoking cessation. When a smoker quits, the quick shift in metabolic rate can transform a previously ineffective dose into one that is too potent. This makes regular follow-ups crucial during periods of smoking reduction or cessation. Medication dosages often need to be tapered or adjusted to account for the body’s changing ability to metabolize drugs. Healthcare professionals must also monitor patients closely for emerging side effects or signs of serotonin syndrome if blood levels of antidepressants rise unexpectedly.
Beyond individual drug interactions, the behavioural and psychological aspects of smoking complicate adherence to antidepressant treatment.Smokers with depression may have lower motivation to follow medication regimens consistently, especially if they perceive little benefit or rely on nicotine as a mood regulator. Missed doses and inconsistent intake can further destabilize their condition and increase the likelihood of relapse. They can even develop symptoms of antidepressant discontinuation syndrome.
In clinical practice, a thorough assessment of smoking habits should be a standard part of prescribing antidepressants. This includes asking about the quantity of cigarettes smoked daily, the duration of smoking, and any plans or interest in quitting. This information is crucial for selecting appropriate medications and anticipating dose adjustments.
Clinicians should also be proactive in educating patients about the impact of smoking on treatment outcomes, which can serve as a powerful motivator for change.
Therapeutic Considerations
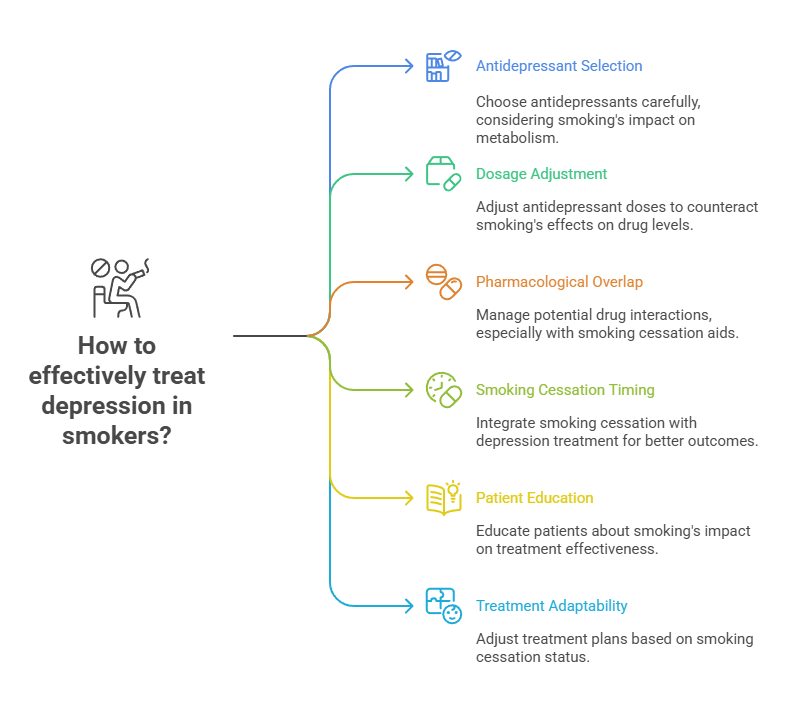
When treating individuals with depression who smoke, a number of therapeutic considerations must be taken into account to ensure effective, safe, and sustainable treatment outcomes.You see, smoking influences antidepressant response and treatment outcomes. These factors then necessitate a personalized approach to treatment that addresses both the psychiatric condition and the behavioural aspects of tobacco dependence.
A primary therapeutic concern is the selection and dosing of antidepressants. Cigarette smoke induces hepatic enzymes, particularly CYP1A2, affecting the metabolism of tricyclic antidepressants and some SSRIs like fluvoxamine. In smokers, these medications may be cleared more rapidly from the body, which leads to subtherapeutic serum concentrations and diminished clinical effectiveness.
Consequently, higher doses of these antidepressants may be required for smokers to achieve the same therapeutic benefits seen in non-smokers. This has been well documented in research examining drug metabolism in smokers, indicating that failure to adjust dosing can lead to under-treatment and persistent depressive symptoms.
Another important therapeutic consideration is the potential for pharmacological overlap or synergy. Pharmacological overlap is a situation wherein different drugs or medicines work in similar ways, target the same body parts, or have similar effects. When these drugs are mixed together, they can create either helpful (synergistic effects) or not-so-helpful (antagonistic effects or more side effects) interactions. For instance, bupropion serves a dual role as both an antidepressant and a smoking cessation aid. Its dopaminergic and noradrenergic action not only relieves depressive symptoms but also helps reduce nicotine cravings. The unique profile of bupropion makes it an appropriate first-line choice for patients motivated to quit smoking while also managing depressive symptoms.
However, care must be taken in patients with a history of seizures or eating disorders. This underscores the significance of conducting a thorough patient history and risk assessment before initiating medical treatment through drugs.
Varenicline, another medical treatment with drugs for smoking cessation, also demands caution. Although it’s not an antidepressant, it’s been widely used for its efficacy in helping patients quit smoking.
Initially, there were concerns about neuropsychiatric side effects like mood changes and suicidal thoughts, particularly in those with pre-existing psychiatric conditions. However, recent studies like the EAGLES trial found no significant increase in neuropsychiatric events among patients with mental illness using varenicline compared to placebo. Despite this reassurance, healthcare professionals are advised to closely monitor patients when varenicline is prescribed alongside antidepressants.
The timing of smoking cessation in relation to antidepressant therapy is also crucial.Starting smoking cessation during an acute depressive episode may seem counterproductive due to concerns about elevating mood instability. But growing evidence suggests that quitting smoking can lead to long-term improvements in mental health, including reductions in anxiety, depression, and stress levels. Integrating smoking cessation efforts with depression treatment, when appropriately timed and supported, can lead to better overall outcomes.
Patient education is another factor that must be considered. Many individuals are unaware that smoking can reduce the effectiveness of their antidepressants. Educating patients about the pharmacokinetic implications of smoking empowers them to actively carry out their treatment plans. It can also serve as a motivational tool for cessation, especially when patients understand that continuing to smoke may hinder their recovery.
Finally, treatment plans must be adaptable.For instance, if a patient who smokes decides to quit during antidepressant therapy, healthcare professionals must anticipate changes in drug metabolism. Smoking cessation can reduce enzyme induction, which leads to increased blood levels of antidepressants. Regular follow-up appointments and therapeutic drug monitoring, when available, can likewise help mitigate these risks and ensure treatment remains both effective and safe.
Therapeutic success requires an integrated care approach that combines pharmacological treatment with behavioural support, patient education, and ongoing clinical assessment. Only through coordinated care can doctors effectively manage the challenges of treating depression among smokers.
Mental Health Considerations
Mental health considerations are necessary to understand the relationship between smoking cigarettes and depression, especially in clinical contexts where both conditions co-exist.Smoking is typically more common among individuals with mental health disorders. This co-morbidity creates unique challenges in terms of treatment and recovery. Addressing the psychological, behavioural, and social factors behind smoking in individuals with depression helps in achieving better clinical outcomes.
Smokers with depression typically use cigarettes to regulate their emotions. They depend on nicotine to temporarily alleviate symptoms like low mood, anxiety, and irritability. The short-term effects of the said substance on neurotransmitters like dopamine and serotonin often provide a perceived mood boost, reinforcing cigarette smoking as a maladaptive coping mechanism.
In the long run, however, nicotine dependence can worsen one’s mental health. Repeated withdrawal and re-administration cycles can contribute to chronic mood instability, increased stress sensitivity, and deeper nicotine dependence over time. This pattern not only sustains depressive symptoms but also makes smokers more resistant to traditional therapies.
One’s attachment to smoking further complicates therapeutic engagement. Those with depression report that cigarette smoking is among the few activities that can give them immediate comfort, making them reluctant to consider smoking cessation. Even the suggestion of quitting smoking may trigger anxiety or boost feelings of hopelessness for some smokers.
With these types of cigarette smokers, clinicians must be sensitive to their psychological dynamics when discussing treatment options. They must also avoid applying undue pressure as it can only damage therapeutic rapport and patient trust.
Smoking may also be tied to identity and social factors. For those living with depression, especially those with limited social support, smoking may serve as a form of social interaction or daily routine that gives structure to an otherwise unmotivated or withdrawn lifestyle. These associations must be acknowledged in care plans. Replacing smoking with positive coping strategies like structured activities, behavioural activation, or social engagement can reduce the psychological resistance to quitting while supporting recovery from depression.
Cognitive function is another key mental health consideration.Chronic nicotine use may lead to subtle cognitive deficits over time, particularly in attention, memory, and executive function. While nicotine can offer short-term improvements in alertness, sustained use of cigarettes often results in diminished cognitive performance once dependence is established.
When depression is also present, these impairments may hinder treatment engagement, decision-making, and medication adherence. Tailored interventions that include cognitive-behavioural strategies and psychoeducation can help patients build self-awareness and adopt healthier behaviours.
The risk of suicide and self-harm in individuals with both depression and nicotine dependence should also be considered. Studies have found higher rates of suicidal thoughts and attempts among smokers with depression compared to non-smokers with the same diagnosis. While the reasons are multifactorial, healthcare professionals must screen for suicide risk more rigorously in this population. Treatment plans should include regular mood assessments and strong safety planning, especially during the early phases of smoking cessation or medication changes.
Mental health stigma presents another barrier to effective intervention.Individuals with depression who smoke may already feel judged for their condition and lifestyle choices. If they perceive further judgment around their smoking, they may become disengaged from care or minimize their nicotine use when speaking with healthcare providers. Validating the patient’s experience while offering realistic pathways to change fosters collaboration rather than resistance.
Finally, integrating mental health support with smoking cessation programs can greatly improve outcomes. Psychological therapies such as cognitive behavioural therapy (CBT) and motivational interviewing (MI) have shown effectiveness in helping individuals with depression reduce or quit smoking. These approaches can target maladaptive beliefs, build coping skills, and enhance motivation in a way that supports both mood stability and behavioural change.
Frequently Asked Questions
What happens when you smoke on antidepressant?
When you smoke while taking an antidepressant, cigarettes can speed up the metabolism of the medicine, making it less effective. This is due to the compounds in cigarette smoke that activate liver enzymes, breaking down medications more quickly. Eventually, you’ll experience weaker symptom relief or require higher doses to achieve the desired effect.
Is it okay to smoke cigarettes while on medication?
While smoking is not outright prohibited while on most medications, it can somehow interfere with how your body processes them. This can reduce the effectiveness of treatment or increase the risk of side effects, especially with drugs metabolized by liver enzymes like CYP1A2.
What is the best antidepressant for smokers?
The best antidepressant for smokers is bupropion. Aside from regulating the effects of depression, it is considered a suitable antidepressant for smokers since it can also help reduce nicotine cravings and support smoking cessation. Over the years, this antidepressant medication has shown an increase in quit rates among smokers while mitigating depressive symptoms.
Summary
While it’s technically possible to smoke cigarettes while taking antidepressants, many studies found that doing so might not be a viable habit in the long run.
Cigarette smoke, which contains nicotine and other harmful substances, can alter how your body processes certain antidepressants. It can potentially reduce the therapeutic benefit of the antidepressants or increase the risk of their side effects. Moreover, smoking cigarettes may worsen depressive symptoms in the long run, which makes recovery more difficult.
If you’re being treated for depression and currently smoke cigarettes, it’s essential that you speak with your healthcare provider. Additionally, you should know the key components of cigarettes as they can give you an insight into how harmful they are. One of these components is tar. Know what is tar in cigarettes here at Native Smokes 4 Less.